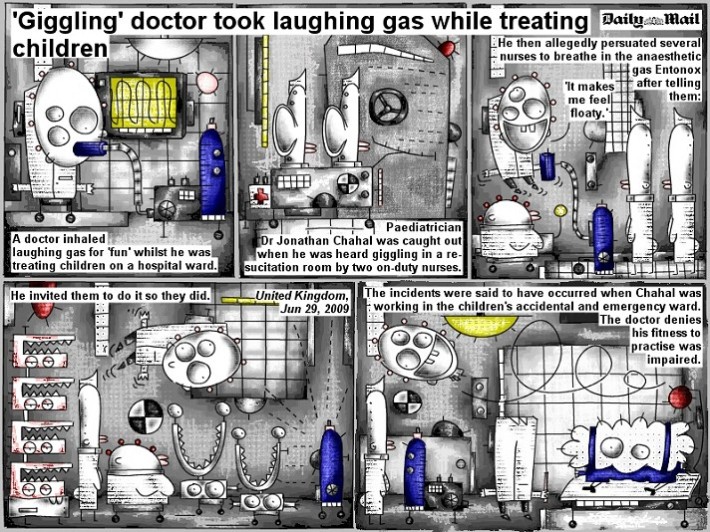
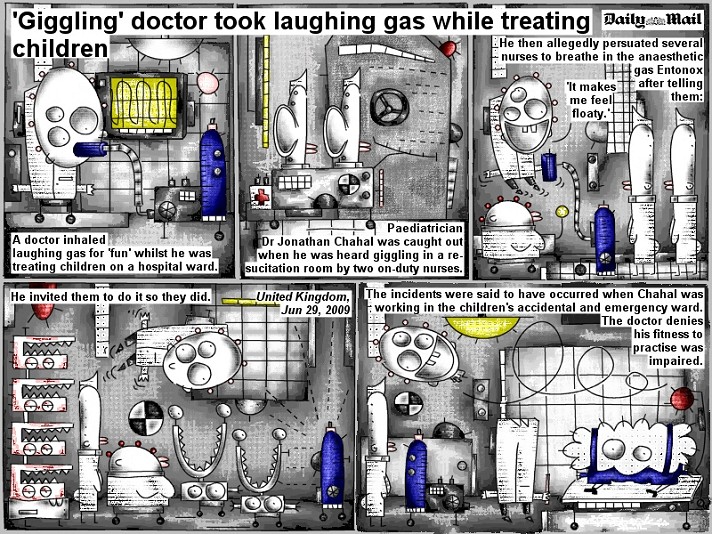
 ‘Giggling’ doctor took laughing gas while treating children
‘Giggling’ doctor took laughing gas while treating children
A doctor inhaled laughing gas for ‘fun’ whilst he was treating children on a hospital ward.
Paediatritian Dr Jonathan Chahal was caught out when he was heard giggling in a resucitation room by two on-duty nurses.
He then allegedly persuated several nurses to breathe in the anaesthetic gas Entonox after telling them: ‘It makes me feel floaty.’
He invited them to do it so they did.
The incidents were said to have occurred when Chahal was working in the children’s accidental and emergency ward. The doctor denies his fitness to practise was impaired.
giggling oder gickerlinge? das wäre auch hier eine frage. aber um einen weiser auf einen artikel ist auch nicht schade. denn die überschrift erinnert mich an bob schroeders titeleien.
A 28-Year-Old With a Fever of Unknown Origin
A 28-year-old woman is transferred from an outside hospital with a chief complaint of fever of unknown origin for the past 3 months. Her fever has been as high as 102.2°F (39°C) and has had no noticeable pattern. The patient has a history of bronchial asthma and chronic bronchitis that has not responded to multiple courses of antimicrobial treatment including amoxicillin/clavulanic acid, cefotaxime, and levofloxacin. She has a 5-year history of asthma managed with inhaled bronchodilators and an occasional need for aminophylline. She also has a history of allergic rhinitis that precedes her history of asthma. Severe upper-back pain that limits movement and is associated with numbness of the sole of her right foot developed 2 weeks after the fever. She has noted difficulty holding heavy objects with either her right or left hand and difficulty with other upper-extremity tasks, such as combing her hair. She has a productive cough (yellowish sputum) that is not related to posture and has no diurnal variation. She reports significant weight loss. Although she is unable to quantify how much weight she has lost, she notes that her clothes no longer fit her. She does not smoke or take other medications, has not traveled, and does not have pets.
On examination, the patient is very uncomfortable and restless. Besides the high fever, she has a pulse of 110 beats/min, blood pressure of 110/70 mm Hg, and a respiratory rate of 25 breaths/min.
The patient weighs about 187 lb (85 kg; this likely represents a nearly 44-lb [20-kg] weight loss over the preceding 5 to 6 months). Examination of the chest reveals crepitations and wheezes throughout both lung fields, but normal heart sounds without evidence of cardiac murmur or friction rub are found. Examination of the back reveals severe tenderness of the midline cervical spine, which broadens to involve both shoulders down the spine to the 2nd lumbar vertebra. Proximal weakness of both upper limbs is noted, but the sensory examination of the upper extremities is normal. Lower extremity sensory motor examination is normal and symmetric.
No cervical, axillary, or inguinal lymph node enlargement is noted. An abdominal examination reveals no tenderness, rigidity, ascites, organomegaly, or masses. Additionally, no lower extremity edema is found, and intact dorsalis pedis, posterior tibialis, and radial pulses are felt.
The laboratory investigations include a complete blood cell count (CBC) with a hemoglobin of 12.9 gm/dL, a platelet count of 350,000/mm3, and a white blood cell count of 25,000/mm3, with 12% eosinophils. The erythrocyte sedimentation rate (ESR) is elevated at 65 in the 1st hour. Liver enzyme findings are unremarkable, with an AST of 35 IU, ALT of 25 IU, and a serum bilirubin of 0.7 mg/dL. The creatinine is normal at 0.5 mg, with a blood urea nitrogen (BUN) of 35 mg/dL. The rheumatoid factor finding is positive. A urine analysis shows no evidence of infection or proteinuria.
A plain chest radiograph is performed (Figure 1), which reveals multiple scattered infiltrates in both lungs. A high-resolution CT scan (Figure 2) shows interstitial lung fibrosis.
nachlesen auf http://www.medscape.org/viewarticle/757309?src=emed_case_nl_0. aber nur, wenn Sie sich einloggen, Monsieur.
Hoffe, habe den faden hier nicht gesprengt.
Hut.
ja die gickerlinge … im märchen gerollt, mit einem liedchen bedacht und nun hier. vom feinsten! sehr schön die farbgebungen und das glänzende gülden … gg … :)